Psycho Audiological Assessment
 What are hearing tests and questionnaires that I should expect when seeing a specialist audiologist for tinnitus/hyperacusis/misophonia rehabilitation?
What are hearing tests and questionnaires that I should expect when seeing a specialist audiologist for tinnitus/hyperacusis/misophonia rehabilitation?
Tinnitus is perception of sound in the ears or head with no acoustic stimulation. People typically describe their tinnitus as a buzzing noise, high-pitched noise, hissing, whistle, waterfall and grinding wheel, ringing, white noise, wind noise, bubbles, clicks, beep, or humming. About 20% of patients are unable to describe what their tinnitus sounds like. Hyperacusis is intolerance to certain everyday sounds that causes significant distress and impairment in social, occupational, recreational, and other day-to-day activities. Intolerance to certain sounds related to eating, lip smacking, sniffing, breathing, clicking sounds, and tapping noises is known as misophonia or annoyance hyperacusis.
All patients should undergo thorough medical evaluation by their physician and ENT specialist prior to be referred for tinnitus and/or hyperacusis rehabilitation.
There are variations in assessment procedures used in different settings. However, the typical psycho-audiological assessment methods used in the process of tinnitus and/or hyperacusis rehabilitation comprise (1) pure tone audiometry (modified version of the BSA, 2011a), (2) Uncomfortable Loudness Levels (ULLs) test (modified version of the BSA, 2011b), (3) assessment of tinnitus and hyperacusis using psychometric instruments, (4) insomnia assessment, and (5) screening of the psychological disorders.
Pure Tone Audiometry

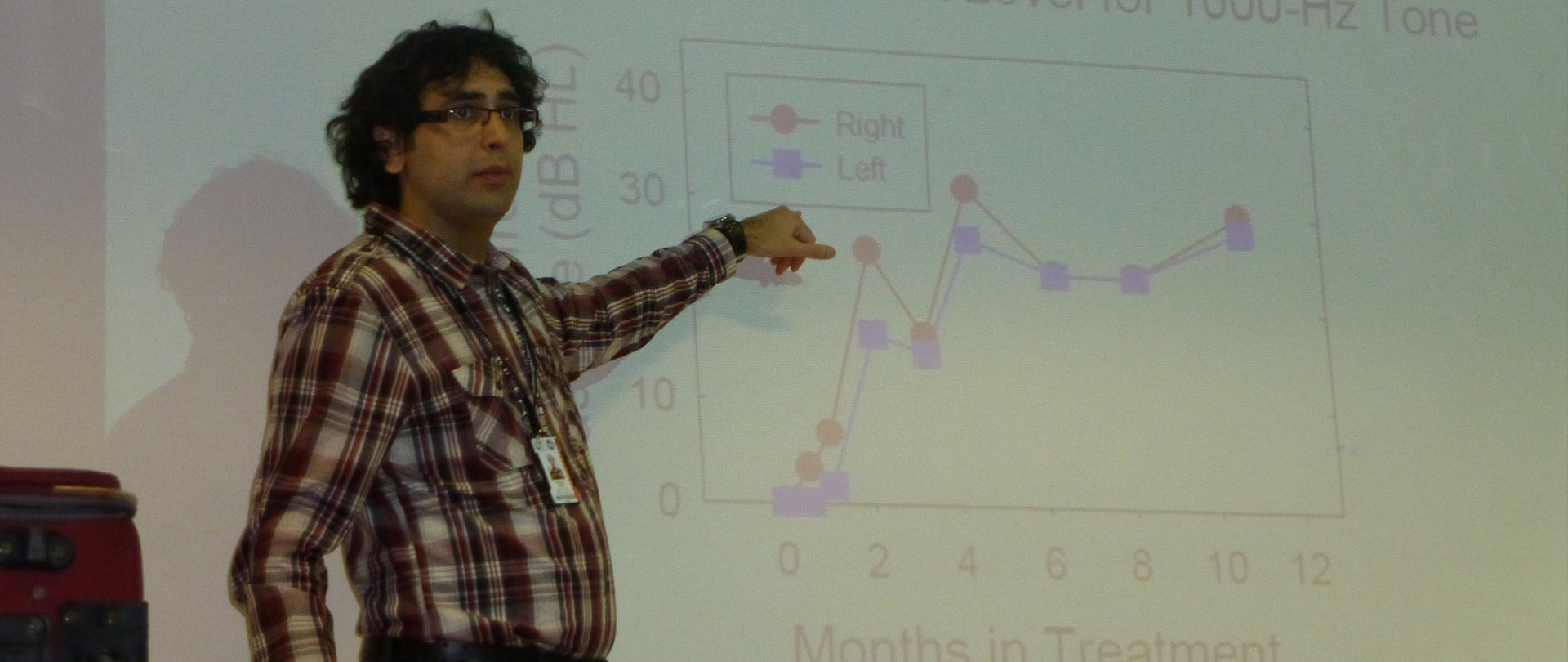
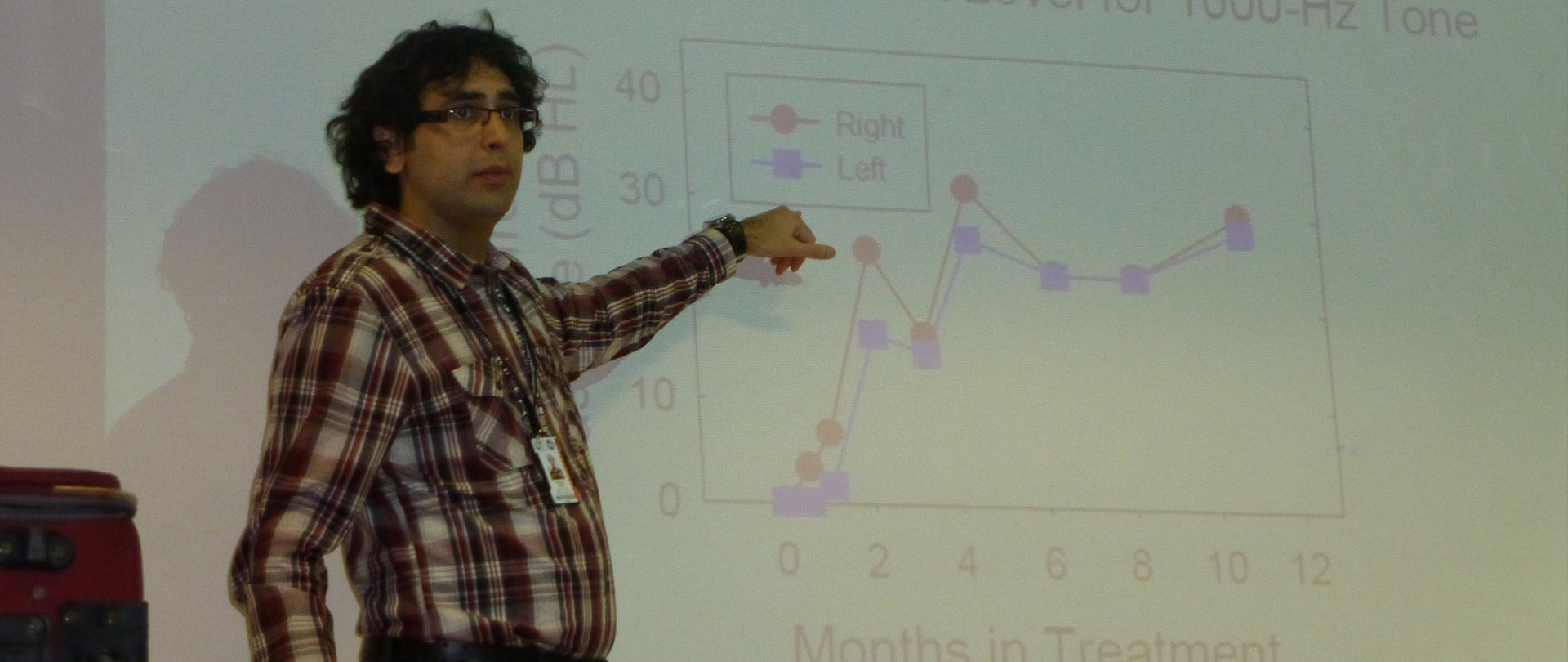
Pure tone audiogram should be measured using the procedure recommended by the British Society of Audiology (BSA 2011a), but with some modifications proposed by Aazh and Moore (2017b) to avoid any discomfort for patients who experiment tinnitus, hyperacusis, misophonia or any type of noise sensitivity. The starting presentation level at 0.25, 0.5, 2, 3, 4, 6, and 8 kHz should be equal to the measured audiometric threshold at the adjacent frequency (e.g., if the threshold at 1 kHz is 20 dB HL, the starting level for measuring the threshold at 2 kHz should be 20 dB HL, instead of 50 dB HL as recommended by the BSA).
Uncomfortable Loudness Levels (ULLs)
ULLs should be measured following the BSA recommended procedure (BSA 2011b), but with the modifications proposed by Aazh and Moore (2017b), to avoid any discomfort. The starting presentation level should be equal to the measured audiometric threshold at the test frequency. In addition, levels above 80 dB HL are not used. If the ULL is not reached at 80 dB HL, the ULL at the test frequency is recorded as 85 dB HL.
The self-report questionnaires
The questionnaires listed below should be applied before the start of the treatment and at the end of the last session. Patients should complete these without involvement of their audiologist.
(1) Tinnitus Handicap Inventory (THI; Newman et al. 1996)
The THI has 25 items, and response choices are “no” (0 points), “sometimes” (2 points) and “yes” (4 points). The overall score ranges from 0 to 100. Scores from 0–16 indicate no handicap, scores from 18–36 indicate mild handicap, scores from 38–56 indicate moderate handicap, and scores from 58–100 indicate severe handicap (Newman et al. 1996).
(2) Hyperacusis Questionnaire (HQ; Khalfa et al. 2002)
The HQ comprises 14 items and the response choices are “no” (0 points), “yes, a little” (1 point), “yes, quite a lot” (2 points), and “yes, a lot” (3 points). The overall score ranges from 0 to 42. Scores of 22 or more should be taken as indicating the presence of hyperacusis handicap (Aazh & Moore 2017a).
(3) Insomnia Severity Index (ISI; Bastien et al. 2001)
Insomnia is associated with difficulty in initiating sleep, maintaining sleep, and/or achieving restorative sleep (McCall 2004). Difficulty in getting to sleep, waking in the middle of the night, and waking early have been reported as the main types of sleep disturbance experienced by tinnitus sufferers (Hallam et al. 1988). The ISI comprises seven items that assess the severity of sleep difficulties and their effect on the patient’s life. Each item is rated on a scale from 0 to 4 and the total score ranges from 0 to 28. Scores from 0-7 indicate no clinically significant insomnia, scores from 8-14 indicate slight insomnia, scores from 15-21 indicate moderate insomnia, and scores from 22-28 indicate severe insomnia (Bastien et al. 2001).
(5) Visual Analogue Scale (VAS; Maxwell 1978) of tinnitus loudness, annoyance and effect on life.
VAS scores are ratings on a scale from 0 to 10. The VAS score for the loudness of tinnitus is assessed by asking the patient to rate the loudness of tinnitus during their waking hours over the last months. The VAS score for annoyance induced by the tinnitus is assessed by asking the patient to rate their subjective perception of annoyance on average during the last month. The VAS score for the impact of tinnitus on their life is assessed by asking the patient to rate the effect of tinnitus on their life during the last month.
(6) Generalized Anxiety Disorder questionnaire (GAD-7; Spitzer et al. 2006).
This is a 7-item questionnaire for assessment of anxiety symptoms. Patients are asked how often during the last 2 weeks they had been bothered by each symptom. Response options are not at all (0), several days (1), more than half the days (2), and nearly every day (3). The total score ranges from 0 to 21. The recommended cut-off score for generalized anxiety in the UK mental health system is a score of 8 or above (IAPT 2011).
(7) Patient Health Questionnaire (PHQ-9; Kroenke et al. 2001).
This is a 9-item questionnaire for assessment of depression. The total score ranges from 0 to 27. The recommended cut-off for caseness for depression in the UK mental health system is a score of 10 or above (IAPT 2011).
References
Aazh, H., & Moore, B. C. J. (2017a). Factors related to Uncomfortable Loudness Levels for patients seen in a tinnitus and hyperacusis clinic.
International Journal of Audiology 56, 793-800.
Aazh, H., & Moore, B. C. J. (2017b). Incidence of discomfort during pure-tone audiometry and measurement of uncomfortable loudness levels among People seeking help for tinnitus and/or hyperacusis
American Journal of Audiolgy,
26, 226-232.
Bastien, C. H., Vallieres, A., & Morin, C. M. (2001). Validation of the Insomnia Severity Index as an outcome measure for insomnia research.
Sleep Med,
2, 297-307.
BSA (2011a).
Pure-tone air-conduction and bone-conduction threshold audiometry with and without masking: Recommended Procedure. Reading, UK: British Society of Audiology.
BSA (2011b).
Recommended Procedure: Determination of uncomfortable loudness levels. Reading, UK: British Society of Audiology
Hallam, R. S., Jakes, S. C., & Hinchcliffe, R. (1988). Cognitive variables in tinnitus annoyance.
Br J Clin Psychol,
27 ( Pt 3), 213-22.
IAPT (2011). The IAPT Data Handbook: Guidance on recording and monitoring outcomes to support local evidence-based practice In D. o. Health (Ed.), UK: IAPT National Programme Team
Khalfa, S., Dubal, S., Veuillet, E., et al. (2002). Psychometric normalization of a hyperacusis questionnaire.
ORL J Otorhinolaryngol Relat Spec,
64, 436-42.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure.
J Gen Intern Med,
16, 606-13.
Maxwell, C. (1978). Sensitivity and accuracy of the visual analogue scale: a psycho-physical classroom experiment.
Br J Clin Pharmacol,
6, 15-24.
McCall, W. V. (2004). Sleep in the elderly: burden, diagnosis, and treatment. .
Prim Care Companion J Clin Psychiatry,
6, 9-20.
Newman, C. W., Jacobson, G. P., & Spitzer, J. B. (1996). Development of the Tinnitus Handicap Inventory.
Arch Otolaryngol Head Neck Surg,
122, 143-8.
Spitzer, R. L., Kroenke, K., Williams, J. B., et al. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7.
Arch Intern Med,
166, 1092-7.
 What are hearing tests and questionnaires that I should expect when seeing a specialist audiologist for tinnitus/hyperacusis/misophonia rehabilitation?
Tinnitus is perception of sound in the ears or head with no acoustic stimulation. People typically describe their tinnitus as a buzzing noise, high-pitched noise, hissing, whistle, waterfall and grinding wheel, ringing, white noise, wind noise, bubbles, clicks, beep, or humming. About 20% of patients are unable to describe what their tinnitus sounds like. Hyperacusis is intolerance to certain everyday sounds that causes significant distress and impairment in social, occupational, recreational, and other day-to-day activities. Intolerance to certain sounds related to eating, lip smacking, sniffing, breathing, clicking sounds, and tapping noises is known as misophonia or annoyance hyperacusis.
All patients should undergo thorough medical evaluation by their physician and ENT specialist prior to be referred for tinnitus and/or hyperacusis rehabilitation.
There are variations in assessment procedures used in different settings. However, the typical psycho-audiological assessment methods used in the process of tinnitus and/or hyperacusis rehabilitation comprise (1) pure tone audiometry (modified version of the BSA, 2011a), (2) Uncomfortable Loudness Levels (ULLs) test (modified version of the BSA, 2011b), (3) assessment of tinnitus and hyperacusis using psychometric instruments, (4) insomnia assessment, and (5) screening of the psychological disorders.
What are hearing tests and questionnaires that I should expect when seeing a specialist audiologist for tinnitus/hyperacusis/misophonia rehabilitation?
Tinnitus is perception of sound in the ears or head with no acoustic stimulation. People typically describe their tinnitus as a buzzing noise, high-pitched noise, hissing, whistle, waterfall and grinding wheel, ringing, white noise, wind noise, bubbles, clicks, beep, or humming. About 20% of patients are unable to describe what their tinnitus sounds like. Hyperacusis is intolerance to certain everyday sounds that causes significant distress and impairment in social, occupational, recreational, and other day-to-day activities. Intolerance to certain sounds related to eating, lip smacking, sniffing, breathing, clicking sounds, and tapping noises is known as misophonia or annoyance hyperacusis.
All patients should undergo thorough medical evaluation by their physician and ENT specialist prior to be referred for tinnitus and/or hyperacusis rehabilitation.
There are variations in assessment procedures used in different settings. However, the typical psycho-audiological assessment methods used in the process of tinnitus and/or hyperacusis rehabilitation comprise (1) pure tone audiometry (modified version of the BSA, 2011a), (2) Uncomfortable Loudness Levels (ULLs) test (modified version of the BSA, 2011b), (3) assessment of tinnitus and hyperacusis using psychometric instruments, (4) insomnia assessment, and (5) screening of the psychological disorders.
 Pure tone audiogram should be measured using the procedure recommended by the British Society of Audiology (BSA 2011a), but with some modifications proposed by Aazh and Moore (2017b) to avoid any discomfort for patients who experiment tinnitus, hyperacusis, misophonia or any type of noise sensitivity. The starting presentation level at 0.25, 0.5, 2, 3, 4, 6, and 8 kHz should be equal to the measured audiometric threshold at the adjacent frequency (e.g., if the threshold at 1 kHz is 20 dB HL, the starting level for measuring the threshold at 2 kHz should be 20 dB HL, instead of 50 dB HL as recommended by the BSA).
Pure tone audiogram should be measured using the procedure recommended by the British Society of Audiology (BSA 2011a), but with some modifications proposed by Aazh and Moore (2017b) to avoid any discomfort for patients who experiment tinnitus, hyperacusis, misophonia or any type of noise sensitivity. The starting presentation level at 0.25, 0.5, 2, 3, 4, 6, and 8 kHz should be equal to the measured audiometric threshold at the adjacent frequency (e.g., if the threshold at 1 kHz is 20 dB HL, the starting level for measuring the threshold at 2 kHz should be 20 dB HL, instead of 50 dB HL as recommended by the BSA).
 ULLs should be measured following the BSA recommended procedure (BSA 2011b), but with the modifications proposed by Aazh and Moore (2017b), to avoid any discomfort. The starting presentation level should be equal to the measured audiometric threshold at the test frequency. In addition, levels above 80 dB HL are not used. If the ULL is not reached at 80 dB HL, the ULL at the test frequency is recorded as 85 dB HL.
ULLs should be measured following the BSA recommended procedure (BSA 2011b), but with the modifications proposed by Aazh and Moore (2017b), to avoid any discomfort. The starting presentation level should be equal to the measured audiometric threshold at the test frequency. In addition, levels above 80 dB HL are not used. If the ULL is not reached at 80 dB HL, the ULL at the test frequency is recorded as 85 dB HL.
 The questionnaires listed below should be applied before the start of the treatment and at the end of the last session. Patients should complete these without involvement of their audiologist.
(1) Tinnitus Handicap Inventory (THI; Newman et al. 1996)
The THI has 25 items, and response choices are “no” (0 points), “sometimes” (2 points) and “yes” (4 points). The overall score ranges from 0 to 100. Scores from 0–16 indicate no handicap, scores from 18–36 indicate mild handicap, scores from 38–56 indicate moderate handicap, and scores from 58–100 indicate severe handicap (Newman et al. 1996).
(2) Hyperacusis Questionnaire (HQ; Khalfa et al. 2002)
The HQ comprises 14 items and the response choices are “no” (0 points), “yes, a little” (1 point), “yes, quite a lot” (2 points), and “yes, a lot” (3 points). The overall score ranges from 0 to 42. Scores of 22 or more should be taken as indicating the presence of hyperacusis handicap (Aazh & Moore 2017a).
(3) Insomnia Severity Index (ISI; Bastien et al. 2001)
Insomnia is associated with difficulty in initiating sleep, maintaining sleep, and/or achieving restorative sleep (McCall 2004). Difficulty in getting to sleep, waking in the middle of the night, and waking early have been reported as the main types of sleep disturbance experienced by tinnitus sufferers (Hallam et al. 1988). The ISI comprises seven items that assess the severity of sleep difficulties and their effect on the patient’s life. Each item is rated on a scale from 0 to 4 and the total score ranges from 0 to 28. Scores from 0-7 indicate no clinically significant insomnia, scores from 8-14 indicate slight insomnia, scores from 15-21 indicate moderate insomnia, and scores from 22-28 indicate severe insomnia (Bastien et al. 2001).
(5) Visual Analogue Scale (VAS; Maxwell 1978) of tinnitus loudness, annoyance and effect on life.
VAS scores are ratings on a scale from 0 to 10. The VAS score for the loudness of tinnitus is assessed by asking the patient to rate the loudness of tinnitus during their waking hours over the last months. The VAS score for annoyance induced by the tinnitus is assessed by asking the patient to rate their subjective perception of annoyance on average during the last month. The VAS score for the impact of tinnitus on their life is assessed by asking the patient to rate the effect of tinnitus on their life during the last month.
(6) Generalized Anxiety Disorder questionnaire (GAD-7; Spitzer et al. 2006).
This is a 7-item questionnaire for assessment of anxiety symptoms. Patients are asked how often during the last 2 weeks they had been bothered by each symptom. Response options are not at all (0), several days (1), more than half the days (2), and nearly every day (3). The total score ranges from 0 to 21. The recommended cut-off score for generalized anxiety in the UK mental health system is a score of 8 or above (IAPT 2011).
(7) Patient Health Questionnaire (PHQ-9; Kroenke et al. 2001).
This is a 9-item questionnaire for assessment of depression. The total score ranges from 0 to 27. The recommended cut-off for caseness for depression in the UK mental health system is a score of 10 or above (IAPT 2011).
The questionnaires listed below should be applied before the start of the treatment and at the end of the last session. Patients should complete these without involvement of their audiologist.
(1) Tinnitus Handicap Inventory (THI; Newman et al. 1996)
The THI has 25 items, and response choices are “no” (0 points), “sometimes” (2 points) and “yes” (4 points). The overall score ranges from 0 to 100. Scores from 0–16 indicate no handicap, scores from 18–36 indicate mild handicap, scores from 38–56 indicate moderate handicap, and scores from 58–100 indicate severe handicap (Newman et al. 1996).
(2) Hyperacusis Questionnaire (HQ; Khalfa et al. 2002)
The HQ comprises 14 items and the response choices are “no” (0 points), “yes, a little” (1 point), “yes, quite a lot” (2 points), and “yes, a lot” (3 points). The overall score ranges from 0 to 42. Scores of 22 or more should be taken as indicating the presence of hyperacusis handicap (Aazh & Moore 2017a).
(3) Insomnia Severity Index (ISI; Bastien et al. 2001)
Insomnia is associated with difficulty in initiating sleep, maintaining sleep, and/or achieving restorative sleep (McCall 2004). Difficulty in getting to sleep, waking in the middle of the night, and waking early have been reported as the main types of sleep disturbance experienced by tinnitus sufferers (Hallam et al. 1988). The ISI comprises seven items that assess the severity of sleep difficulties and their effect on the patient’s life. Each item is rated on a scale from 0 to 4 and the total score ranges from 0 to 28. Scores from 0-7 indicate no clinically significant insomnia, scores from 8-14 indicate slight insomnia, scores from 15-21 indicate moderate insomnia, and scores from 22-28 indicate severe insomnia (Bastien et al. 2001).
(5) Visual Analogue Scale (VAS; Maxwell 1978) of tinnitus loudness, annoyance and effect on life.
VAS scores are ratings on a scale from 0 to 10. The VAS score for the loudness of tinnitus is assessed by asking the patient to rate the loudness of tinnitus during their waking hours over the last months. The VAS score for annoyance induced by the tinnitus is assessed by asking the patient to rate their subjective perception of annoyance on average during the last month. The VAS score for the impact of tinnitus on their life is assessed by asking the patient to rate the effect of tinnitus on their life during the last month.
(6) Generalized Anxiety Disorder questionnaire (GAD-7; Spitzer et al. 2006).
This is a 7-item questionnaire for assessment of anxiety symptoms. Patients are asked how often during the last 2 weeks they had been bothered by each symptom. Response options are not at all (0), several days (1), more than half the days (2), and nearly every day (3). The total score ranges from 0 to 21. The recommended cut-off score for generalized anxiety in the UK mental health system is a score of 8 or above (IAPT 2011).
(7) Patient Health Questionnaire (PHQ-9; Kroenke et al. 2001).
This is a 9-item questionnaire for assessment of depression. The total score ranges from 0 to 27. The recommended cut-off for caseness for depression in the UK mental health system is a score of 10 or above (IAPT 2011).